Can Pelvic Floor Exercise Help With Low Back Pain?
March 11, 2024

Low back pain is one of the most common health challenges in the world. The WHO estimates that over 600 million people globally experience low back pain, and it is the leading cause of disability in the entire world. Furthermore, it is becoming more common (the number of sufferers is estimated to increase by more than 30% by 2050) and it produces an enormous economic burden since it frequently causes substantial quality of life and productivity declines for those who experience it.
So, there’s clearly a LOT of motivation to understand the best ways to treat and prevent low back pain. Acknowledging that it is a complex condition that can have many and varied contributing factors, research has been published recently that looks at pelvic floor exercise as one potential tool that can be quite effective. Given our interest in pelvic floor fitness, we wanted to dig into that research and share some thoughts on the value (and limitations) of pelvic floor exercise as a means to help with low back pain. Read on or skip to the conclusions
Low Back Pain 101
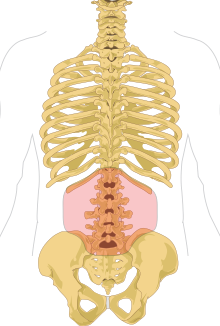
Low back pain is kind of an umbrella definition for any pain occurring between the bottom of the ribs and the buttock on the back side of one’s body – this is also called the “lumbar region”. As the name implies, the main symptom is pain but even then, it can take a lot of forms. Some people experience sharp / shooting / stabbing sensations, whereas for others it can be more of a dull ache. Regardless of what form it takes, the pain can have a number of problematic side effects including stiffness, spasms, or difficulty with movements including standing, walking, sitting, or picking up objects. The pain can also be “acute” (which means it lasts a few days to a few weeks) or “chronic” (which means it lasts at least 3 months and often much longer).
What causes low back pain?
There are MANY different things that can cause low back pain, and even worse is that it can sometimes be idiopathic (which means it arises spontaneously, or at least has no cause that doctors are able to identify).
In cases where there is some cause that can be identified, there is often some sort of injury, condition or disease, especially to the muscles and tendons in one’s back. Common culprits include:
- Overuse, including lifting too much weight or lifting heavy things too frequently
- Posture / ergonomic issues, such as extended sitting or lying down in one position, sleeping in uncomfortable positions, etc
- Arthritis or other degenerative conditions
- Disc problems, such as bulging, torn/herniated, or degenerating discs
- Fractures, for instance from a fall or accident
The above is just a partial list but there are many other factors which can play a role.
What is the current state of the art for treating (or preventing) low back pain?
Because low back pain covers such a broad collection of symptoms and causes, there is no single approach for fixing or preventing it (although on the prevention side, there are some best practices which are fairly universally applicable).
 Exercise can be an effective tool for prevention or treatment of low back pain.
Exercise can be an effective tool for prevention or treatment of low back pain.
Instead, different tools or options may be more effective for different cases. Again here, our intent is not to provide a comprehensive summary of every single treatment option that’s out there, but rather to give a quick overview of some of the more common way stations on a patient’s journey. Broadly speaking, there is often a progression starting with more conservative options and moving towards more powerful, but sometimes more problematic, tools if the “easy” fixes don’t do the trick. That progression may look like:
- Rest: often, activity or even some level of exercise can be very helpful but especially for acute lower back pain with a specific trigger, some rest at the beginning can give your body the chance to reduce inflammation and start healing.
- Physical therapy and exercise: this is particularly effective when the low back pain is caused by musculoskeletal injury but can be extremely useful in other scenarios as well (and exercising the back and abdominal/core muscles is a powerful preventative measure). Furthermore, generally speaking there is a minimal side effect profile for exercise and physiotherapy, which is another advantage.
- Wellness care including massage, acupuncture, chiropractic, etc: as with physical therapy / exercise, these types of treatment modalities can be both preventative or reactive and also have a low side effect profile.
- “Light” medications: over-the-counter nonsteroidal anti-inflammatory drugs (also known as NSAIDs – think ibuprofen) are another extremely common and fairly conservative approach. These don’t do too much as far as addressing the underlying causes but they can help mitigate the pain while the body heals itself.
- More aggressive pharmaceutical treatments: stronger, prescription-based painkillers can also be used, or steroid injections to try to reduce irritation of nerve roots and inflammation in the back.
- Surgery: most appropriate as a last resort because there are potential non-trivial side effects, there are a number of types of surgery that seek to address different underlying causes of low back pain.
Where Does The Pelvic Floor Come In?
There is strong evidence of a link between low back pain and the pelvic floor, from multiple perspectives.Anatomy
The pelvic floor muscles and ligaments all attach, either directly or indirectly, to the tailbone, which is a connection point to the lower back anatomy. Furthermore, the pelvic floor muscles contribute significantly to core strength, stability and function, which can also be related to low back pain (a weak core requires more work from the back, which can cause problems).
In particular, pelvic floor muscles that are too tight or hypertonic (also sometimes referred to as being high tone, or overactive) can pull the sacroiliac joints out of alignment, which can cause low back pain.
Research
To start with, a number of studies have found suggestions that low back pain and pelvic floor function may be connected. For instance, this study from 2018 found that 95% of the participants who were experiencing lumbopelvic pain also had pelvic floor dysfunction.
However, additional research has gone even further in terms of starting to establish causality (not just correlation) and even look at whether pelvic floor exercise can help improve low back pain.

For example, this study from 2020 concluded that “exercises to strengthen the pelvic floor muscles combined with conventional treatment… can provide better outcomes as compared to conventional treatment alone in patients with chronic low back pain.” (Interestingly, they also found that exercises for postural control combined with conventional treatment was more effective than conventional treatment alone).
And this meta-analysis from 2023 that examined the results of 19 individual other studies concluded that “pelvic floor muscle-strengthening exercises significantly reduce low back pain intensity” and that pelvic floor exercise can be regarded as part of a low back pain management plan.
OK, what does it all mean?
There is clear evidence that pelvic floor exercise can be *a* piece of the puzzle as far as trying to address low back pain and the underlying causes. However, it’s important to not confuse that with concluding that pelvic floor exercise is some kind of magic potion, or the only/best/etc weapon at one’s disposal.
We talked above about how low back pain (especially chronic low back pain) is complex and can have many different causes or contributing factors. That means that a diverse arsenal of tools and techniques to deal with low back pain will likely remain necessary forever. But especially in light of the fact that the pelvic floor and how to manage it are not the most well-known aspects of health out there, it’s worth highlighting that adding some pelvic floor exercise to your regimen might be worth considering if you are interested in preventing or treating low back pain.




